Free Sleep Apnea Evaluation
The Process Starts Like This...
Once you get in touch with us, we put you in direct contact with our knowledgeable New Patient Coordinator who can answer many of your questions and help you understand our diagnosis and treatment process. Our New Patient Coordinator also helps us qualify you initially for our comprehensive examination assessment. Once an appointment with Dr. Chapman is scheduled, we will provide you with a comprehensive intake questionnaire that is designed to help us understand the clinical scope of your sleep breathing disorder. This questionnaire is administered through our secure HIPAA compliant portal and helps us start to assess you early on.
On the day of your in-office assessment, several non-invasive tests will be performed to help us determine if we can help you with your sleep apnea. We assess posture and stance and look for signs of wake breathing adaptation that are associated with atlas-axis malpositions. This is important because atlas-axis malpositions can adversely affect the nerves that prevent the upper airway from collapsing while sleeping. We determine if there is functional leg-length discrepancy, and exa mine the spatial orientation of your head, neck, face and jaw system–all of which impact the upper airway. If the findings are positive, then we acquire special 3-D upright images which allow us to definitively measure craniocervical relationships and most importantly, detect airway impingement. The status of the jaw joints may be determined objectively, at this time.

If findings are positive, and no contraindications are detected, you are a candidate for the TAP procedure, and a treatment plan will be presented to you. When you proceed with treatment you will be scheduled for a special in-home sleep study that detects oxygen drops (desaturations), obstructions and correlates these with any clenching or grinding of your teeth at the moment the oxygen drops. There is no catch to it–in fact, we won’t accept you as a sleep apnea patient if we don’t think we can help you.
I have over 27 years managing and treating complex head, neck and jaw disorders and I understand how dysfunction and malalignment of the craniovertebral structures can affect the upper airway. There is a methodology to identify individuals who will likely respond well to treatment and those who won’t. The system is not perfect, but very accurate with over a 95% success rate when we look at treatment outcomes. That is why I invest my time, clinic resources and staff time upfront to make this initial determination. It helps us understand “why” you suffer from sleep apnea. Only if I genuinely feel that I can help you, will I offer you a comprehensive treatment plan. You will not receive a bill from from my office for these services up to this point if you do not chose to proceed with treatment.
One critical part of our examination is to detect a key sign of pharyngeal insufficiency. Specifically, to measure the most constricted point of the pharynx at the minimal cross sectional area. This is the region where 99% of all obstructions occur in obstructive sleep apnea! Below is an example of the immediate changes that occur after we identify a problem that falls within our expertise. The example below is a patient who suffered from a insufficient pharyngeal cross section area of 151.2 mm squared before the TAP, then after performing the TAP procedure, the minimal cross section immediately opened to 267.1 mm squared! Doubling the minimal cross sectional area translate into a 4 fold increase in flow capacity! This is a key measurement that is performed both before and after the TAP procedure. Increasing the resting area of the pharynx translates into a more capacious airway by improving the “tone” of the pharyngeal muscles. That means more oxygen gets into the body, and carbon dioxide does not build up in the tissues. This improvement in tone is there when awake, or asleep. Therefore this patient no longer needed continuous positive air pressure (CPCP) to blast air through a small corridor in order to sleep-breathe!
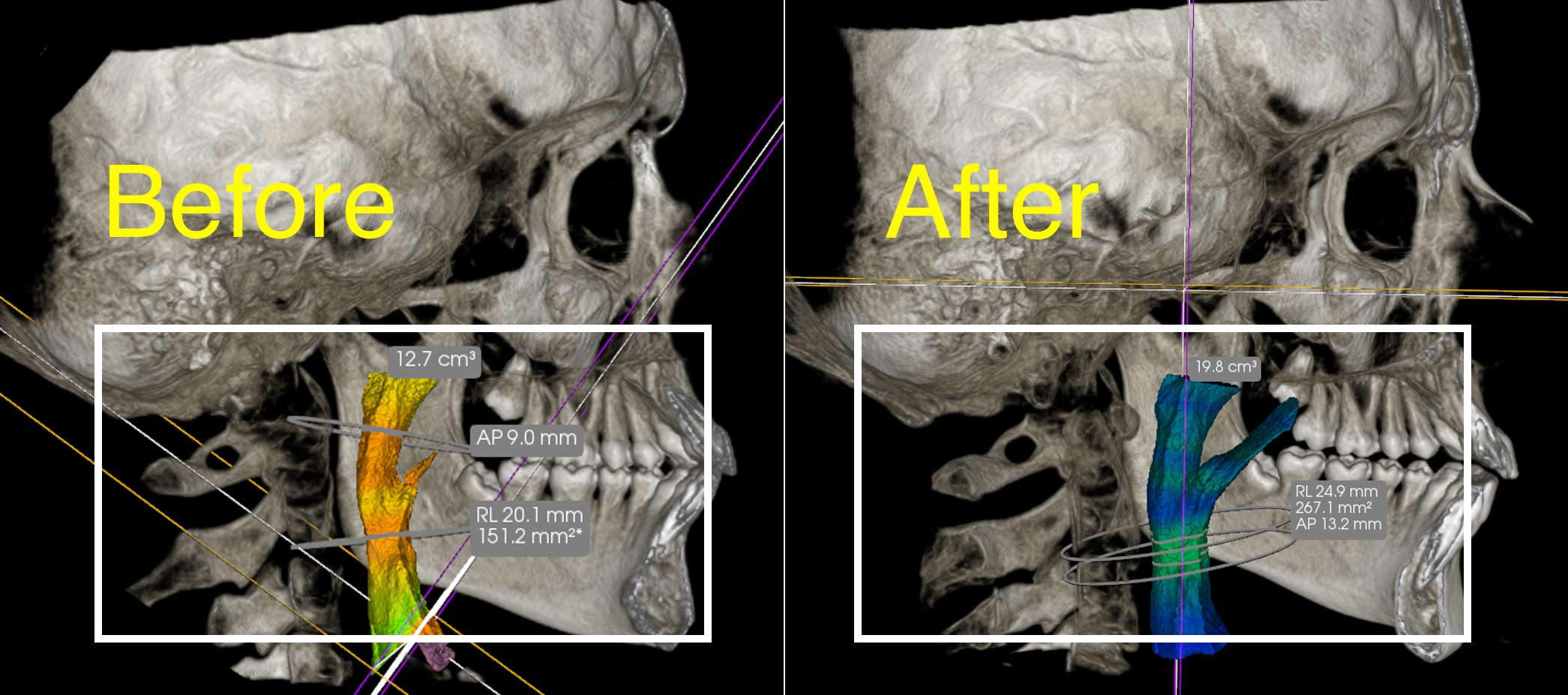
An important note about these images. The “after” image was not performed on the initial assessment visit, but was performed immediately following the TAP procedure which is only performed after acceptance of the treatment plan. In addition to improved airway flow, the most common side benefits are jaw-joint posture changes, improvement to the alignment of the head and neck junction, and better blood flow to and from the brain.
When we complete the TAP procedure, we compare your after-TAP 3-D images to your before-TAP images to make sure we get the changes we want to see. This directly correlates to breathing. It’s a matter of physics, in the sense that a larger diameter airway means better breathing with less resistance. Better breathing means better sleep. Since quality of sleep is tied to longevity and neuro-protectivity in a hundred different ways, better sleep means better life!
Learn more about our Sleep Apnea Treatment
Request Consultation
Fill this out and we will be in contact with you
"*" indicates required fields