“I hate waking up feeling rested and refreshed”, said no one, ever!!
I have never met a soul who has confided in me that they hate a good sleep. On the contrary, when someone sleeps well, it shows in every aspect of their disposition. Why, because there is nothing quite as satisfying as a good, recuperative night’s rest. Who hasn’t lamented that intrusive sound of a blaring, beeping alarm clock, signaling the premature end of a slumber that didn’t quite cut the mustard? Who hasn’t thought to themselves in that moment, “If only I could get a few more hours in before I have to get up..?”
We love sleep because it makes us feel good when we get good quality sleep! But sleep is one of our brain’s most complex functions. I like to compare sleep to an airplane being set on autopilot. When all of the systems are working, autopilot can do 99% of the work over an 8- hour journey or more. Sleep is like this in many ways. When it is working correctly, the brain and body take a restful and recuperative journey through time on a nighttime journey towards recovery, health, and repair from the previous wear and tear caused by the recent awake hours.
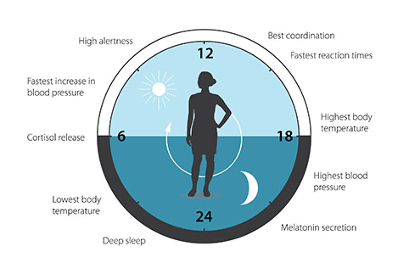
Researchers have discovered that certain genes regulate our sleep. These genes also function in complex ways to “geolocate” us on the planet. In a 2017 Nobel prize press release honoring the 3-way Nobel prize winners doctors Hall, Rosbash and Young proved that “Life on Earth is adapted to the rotation of our planet”, and that we “have an internal, biological clock that helps us anticipate and adapt to the regular rhythm of the day (and night). With exquisite precision, our inner clock adapts our physiology to the dramatically different phases of the day. The clock regulates critical functions such as behavior, hormone levels, sleep, body temperature and metabolism.” Sleep’s auto-pilot programs work largely do to these genes.
https://www.nobelprize.org/prizes/medicine/2017/press-release/
Disordered Breathing Disturbs Sleep
Another autopilot function of the body is breathing, and it can’t be overrated, and it should not be overlooked in your health. When we stop doing it, we die. Thankfully, we don’t have to consciously think about breathing to breathe—it is just something that our body does naturally. It is no surprise to find that good undisturbed breathing is a key part of “good, healthy sleep”. Research has shown that when our breathing is disturbed, so is our sleep, and when our sleep is chronically disturbed, it can affect our brains in both the short and long term. Not only can it affect our energy levels, but it commonly affects our mental health, our productivity, and even our most precious relationships.
There are several types of disturbed sleep associated with events where the body stops breathing. These episodes are called apneic events. There are two main types of apnea, “central” and “obstructive”. Obstructive is where a part of the upper airway (soft palate, tongue or throat muscles lose tone, and collapse in on the airway closing it off partially or completely.) Central apnea is more complicated in that the brain shuts off and restarts breathing at intervals. A third type of apnea combines the two. Recent research suggests that some people with obstructive sleep apnea develop central sleep apnea as a result of using CPAP machines. –Mayo Clinic, Jun 25, 2019
Obstructive Sleep Apnea (OSA)
What is obstructive sleep apnea? This obstructive type of apnea results from “loss of tone” in the smooth muscles that we use to swallow, speak and breath—and for airway protection. These tissues are governed by specific cranial and upper cervical spinal nerves which arise off of the brainstem and upper spinal cord. These nerves allow and provide for the organized and health function of the pharynx. Most obstructive sleep apnea events occur in the mid-section of the pharynx called the oropharynx. In a bit more detail, the front boundary of the oropharynx is the back of the tongue and soft palate, and rear boundary is made up on the atlas lateral mass and the vertebral body of the axis vertebra. The functional space of the pharynx is created and maintained by the healthy and positional status of these structures. When obstructions occur, respirations or ventilation is disturbed. Since inspiration is the number one generator of the pressure gradient that pulls spinal fluid into the head, and draws venous blood out of the head through the internal jugular veins, obstructive breathing can contribute to congestion of the intracranial clearing system known as the glymphatic system. Long term disruption of spinal fluid dynamics can cause early degeneration of the brain by allowing the beta amyloid and tao proteins to congest in the brain tissue.
Obstructive Sleep Apnea Discovery
In over 700 CBCT scans taken of patients diagnosed or suspected of having obstructive sleep apnea, over 90% where observed to have significant rotations of their atlas and axis vertebrae to a point where it encroached on the pharynx. This mechanical fixation measurably diminished the minimum cross section enough to constrict up to 75% of the flow of oxygen.These scans were taken in a normal upright position with the patient centered and standing for the tomogram. Next to CPR neck positioning, upright posture is thought to me the most airway optimized breathing posture. When we lie on our back or side, pharyngeal obstructions become more prevalent. This is particularly the case with back sleepers. In the majority of cases, it is observed that obstructions are intensified by posterior vertebral encroachment on the “soft tube” as the atlas and axis rotate their masses and elements into the compliant pharynx. Our image guided, non-surgical method is shown to expand and increase the restricted flow area by up to 300%, not only measurably improving sleep breathing but solving chronic neck, head and jaw pain.
Unlike obstructive sleep apnea, central apnea is more complicated in that the brain shuts off and restarts breathing at intervals. The areas involved in this disturbed sleep breathing condition is thought to involve the complex region known as the Nucleus Tractus Solitarius (NTS) and is pH reflexive. A third type of apnea combines the two. A 2019 Mayo Clinic study suggests that some people with obstructive sleep apnea develop central sleep apnea as a result of using CPAP machines. (Mayo Clinic, Jun 25, 2019)
Obstructive Sleep Apnea is Harmful to our Health
The long-term effects of sleep apnea can be far reaching and touch every aspect of our lives. Aside from affecting our state of alertness and functioning during the waking hours after a restless night sleep, it can affect our personal relationships and work life. If left untreated, sleep apnea can increase our risk of health problems, including; headaches, worsening ADHD, depression, diabetes, high blood pressure, stroke, and heart failure. It has also been linked to obesity and loss and degeneration of brain matter. It is not a problem to be taken lightly.
The most common treatment of choice for sleep apnea is a continuous positive airway pressure device (CPAP) or a BiPAP. CPAP is a mask that fits over the nose and/or mouth and gently blows air into the airway to help keep it open during sleep. It is this continuous in-blowing of air into the body of someone diagnosed with obstructive sleep apnea that some researchers feel triggers the cascade of reactive neurological patterns that lead to central apnea. A BiPAP is the industries attempt to “normalize” the flow by altering the pressure gradients to allow CO2 to more easily flow out against the influx of air.
The problem with CPAP is that it only treats sleep apnea as a symptom and does nothing to treat the cause of the sleep apnea. It is a lifelong treatment plan, without a cure or improvement over time. In fact, prolonged CPAP use can lead to other disorders as in the most recent recall of machines that allowed filtration material to escape the filter and enter the patient’s lungs, harming respiration rather than help it.
A Cutting-Edge Alternative Sleep Apnea Treatment
Here, we have to discuss a region of the central nervous system that governs the muscles of your pharynx, and therefore provision the patency that allows for the unimpeded flow of gases, CO2 out and O2 in. When the neurological tone to those muscles are unhealthy, the tissues that they control become weak and saggy, collapsing in on the pharynx instead of maintaining its boundaries. This results in the serious health problem we diagnose as obstructive sleep apnea. The part of your central nervous system that operates and protects your upper airway is called the nucleus tractus solitarius, or NTS for short. This vital center coordinates speech, swallowing and breathing. But it is widely agreed that its’ most important function is to Protect the Airway! In a neurological nutshell, the NTS participates and coordinates movements and function of the tongue, the soft palate, chewing and swallowing muscles, the diaphragm, the epiglottis, the heart and lungs. When it is not functioning properly, it can reduce size and interfere with the function of the throat, as well as the downstream organs and systems. The heart, bronchial and gastric systems can pay the price in both the short and long term.
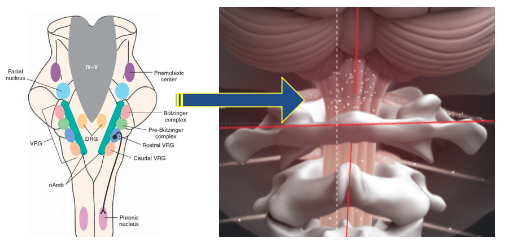
Nucleus Tractus Solitarius receives its’ blood supply from the vertebral arteries which can become twisted and compressed as they course through this mobile and vulnerable region.
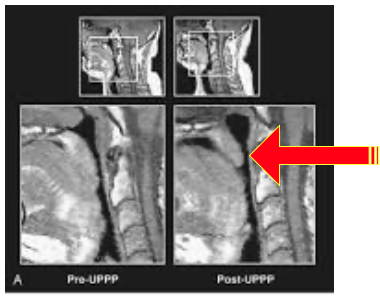
Changes in the pharynx are immediately detectable on CBCT following the Lift Clinic’s innovative new approach to non-invasively correcting pharynx insufficiencies. A TAP procedure using the same technology that miraculously changed storied 1984 Chicago Bears Super Bowl champion Jim MacMahon’s headaches and depression also unlocks these vertebrae and opens channels that affect sleep and breathing centers and also meter spinal fluid flow to and from the head.
This case shows an immediate increase in the upper airway.
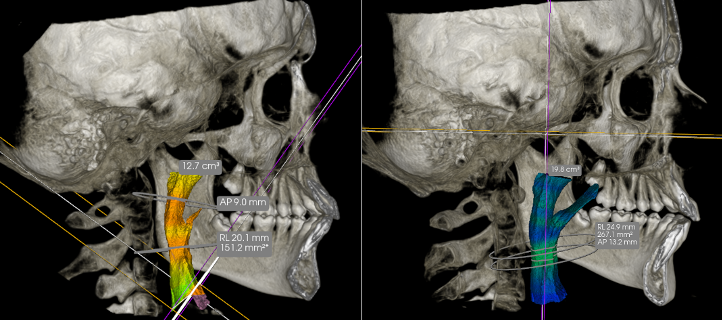
Minimal Cross Sectional improvement Increases Breathing Capacity by over 200% on first TAP Procedure!
The image comparison you see above shows the patient on the left before our alternative sleep apnea treatment in Salt Lake City, and immediately following it. The constriction point in her pharynx increased from 151.2mm2 to 267.1! This was an immediate and permanent change.
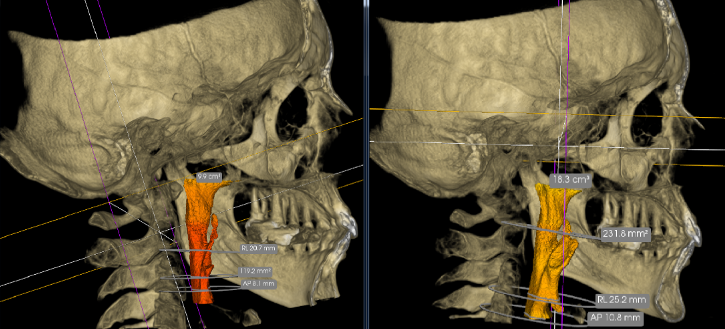
In this case, the minimal cross sectional area increased from 119.2 millimeters squared to 231
There are no downsides to this procedure. It is a closed, image-guided procedure and as you can see in these two recent examples, dramatic changes in upper airway space are real and immediate. The patients instantly felt better and could breathe better–and we could show them why and how. That’s the exciting part of this work, is we get immediate “proofs” of the changes of our alternative sleep apnea treatment in Utah with our imaging tools!
Over the last decade, I have performed this alternative sleep apnea treatment in Salt Lake City thousands of times and obtained measurably increased airways in the majority of my cases.
Ask yourself, why would you undergo risky, invasive surgery or resign yourself to a life-sentence of using a C-PAP or BiPAP before you tried our novel, safe and affective approach? We get to the root of the problem by optimizing blood flow and nutrient delivery directly to the sleep and breathing centers in the central nervous system!
Schedule with us for a complimentary consultation, and take the first step towards getting a restful, rejuvenating sleep. Stop the obstructive sleep apnea caused degenerative process that is going on in your heart, your vascular system and your brain by restoring healthy night-time sleep breathing.
Complex, In-depth and Complimentary
The Lift Clinic offers an initial consultation with diagnostic CT scans if warranted. We can quickly assess your upper cervical spine and craniocervical junction status and your upper airway using images generated by our novel imaging modalities. Before you commit to a lifetime of sleeping with a mask or having risky surgery, schedule a consultation and learn why we have an over 85% positive outcome for our patients.
Continue reading below if you still think sleep apnea surgery is your best best and only option…
A quick Google search of “sleep apnea” and you will find ten common CPAP alternatives for the apneic patient, 8 of them are surgical. I review those 10 options and point out important UPSIDES and DOWNSIDES to those procedures which are mostly surgical. Ultimately though, none of the discussed treatments address the cause of the problem and can be a bit extreme and invasive in their treatment.
TOP TEN THINGS ON GOOGLE SEARCH FOR SLEEP APNEA TREATMENTS!
Side Sleeping
- UPSIDE: Minimally invasive. No surgery or drugs required. May reduce obstructive sleep apnea. Recent studies show improved spinal fluid movement.
- DOWNSIDE: It can be painful on the shoulders, jaw joints and hips. The body can easily turn into a face down posture which is rough on the neck.
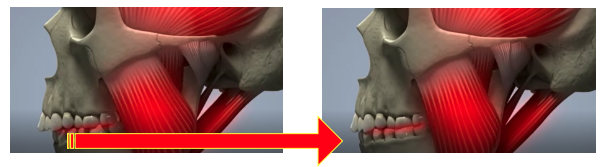
MAD. Mandibular Advancement Device. This is an intraoral appliance that draws the jaw forward, mechanically opening the upper airway.
- UPSIDE: This device works by moving the jaw forward, which increases the size of the upper airway and reduces air resistance behind the soft palate and tongue which can contribute to obstructive sleep apnea and snoring. It may be effective for some patients, especially those with mild or moderate OSA. May reduce obstructive sleep apnea.
- DOWNSIDE: When the jaw is held forward night after night for months, the jaw joints remodel to that advanced position and the bite changes permanently, often requiring more invasive dentistry to resolve—like total mouth restorations costing tens of thousands of dollars. It can also affect the aesthetics of the patients by giving them a “Bulldog” type of a bite. Who doesn’t love a bulldog?
3. Tonsillectomy or Adenoidectomy Surgery. Sometimes if something is infected or inflamed, “conventional wisdom” suggests just getting rid of it. This “throw-away” mentality sells patients short in too many ways to list—but for starters, if the tonsils and adenoids are enlarged, instead of pulling them out and tossing them in the parts bin, let’s figure out what might be causing the inflammation and enlargement. Food and environmental allergies are very common.
- UPSIDE: Instant functional space, and more upper airway volume. May reduce obstructive sleep apnea.
- DOWNSIDE: To get this space you will need to remove a key part of your craniofacial immune system which provides protection for the sinuses, throat, mouth, neck and face. Both your tonsils and adenoids help to trap pathogens, such as bacteria or viruses, that enter your mouth or nose. They contain immune cells that produce antibodies that kill these pathogens before they can spread to the rest of your body.
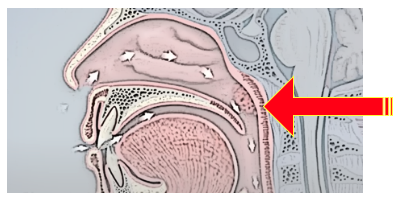
4. Uvulectomy (Removal of the Uvula) Some patients can have a long palate shortened with a procedure known as a UP3 (uvulopalatopharyngoplasty) or uvulectomy — a procedure used to remove excess tissue in the soft palate to widen the airway and allow air to move through the throat more easily. The thought here is exactly the same as removing tonsils, except the uvula does not perform any known immune function. It is, however, a mechanical structure that is key to the function of swallowing, phonation and airway protection. Not only does it “syphon” the sinuses, and help move fluid from the back of the nose into the nasopharynx, it also protects the airway in much the same way that a goalie protects the net.
- UPSIDE: This reduces snoring in roughly 60% of the cases and may be effective in mild to moderate cases of OSA. May reduce obstructive sleep apnea.
- DOWNSIDE: Many people report swallowing dysfunction, choking, pain in throat, nasal regurgitation, and voice change. (Who wants your hockey teams keeper sitting in the box rather than in front of the net?)
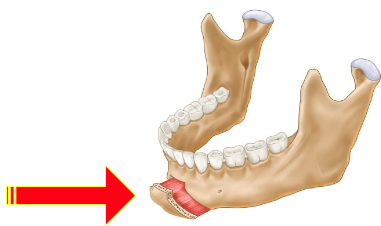
5. GGA (genioglossus advancement) When the airway collapses behind the tongue, a GGA (genioglossus advancement) may be recommended. The surgical procedure is designed to move a portion of the chin bone forward, thereby pulling the base of the tongue muscles forward to increase airway size.
- UPSIDE: This procedure can pull the tongue up and out of the throat and is a relatively simple surgery. Few surgical complications are described in the literature. May reduce obstructive sleep apnea.
- DOWNSIDE: May affect the muscles used for swallowing and the many other muscles associated with tongue posturing. Potential for post-surgical infection and damage to canine roots injury. Permanent tooth numbness or death. Chin and lower lips numbness. Change in appearance. Structural weakening of the lower jaw. Need for additional procedures.
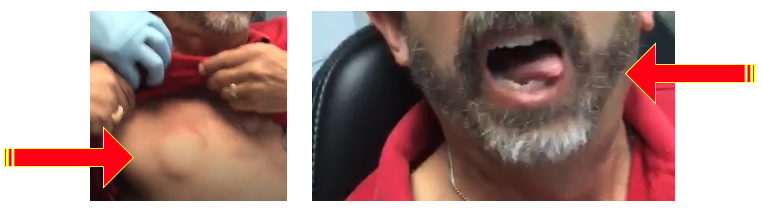
6. Inspire hypoglossal nerve stimulator: Those with a backward collapse of the tongue, diagnosed via a nasal endoscopy, can also be treated using an Inspire hypoglossal nerve stimulator. This consists of a breathing sensor and a stimulation lead powered by a small battery. Implanted during a short outpatient procedure, the device continuously monitors a recipient’s breathing while he or she sleeps. It delivers mild stimulation to key airway muscles and moves the tongue and other soft tissues out of the airway to enable breathing during sleep.
- UPSIDE: Moves the tongue out of the airway and can be useful where one is CPAP intolerant. May reduce obstructive sleep apnea.
- DOWNSIDE: First, it’s expensive. I am aware of one surgery costing nearly $120,000! A hockey puck sized controller is installed on the chest just below the collar bone. Wires are installed on the chest wall in front and back. A stimulator lead is installed on one of the two genioglossus muscles forcing the tongue to protrude more to one side than the other. This is a surgically induced, off-center tongue thrust, which will over time interfere with your bite, tooth position and irritate the tongue (see below). Oh, and if your battery’s die—it stops working!
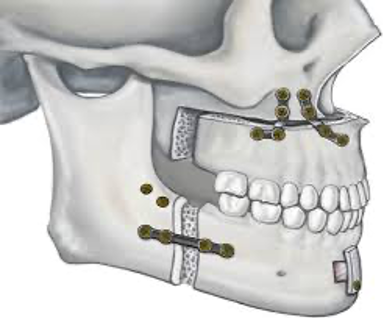
7. MMA surgery (maxillomandibular advancement): Patients with shortened or underdeveloped upper or lower jawbones may benefit from MMA surgery (maxillomandibular advancement), in which the upper jaw (maxilla) and the lower jaw (mandible) are lengthened and moved forward. This surgery is reserved for patients with moderate to severe OSA.
- UPSIDE: In severe underdeveloped jaw situations, it can improve facial aesthetics. When all else fails, try this. May reduce obstructive sleep apnea.
- DOWNSIDE: The most common complications detailed in previous studies are atelectasis, pulmonary embolism, dysrhythmia, hypoxemia, hypotension, chest pain, myocardial infarction, loss of sensation on the face, post-operative pain syndrome and death.
8. MME (maxillomandibular expansion): When a patient’s jawbones are narrow, or long enough but their OSA is severe, the jawbones may be widened using MME (maxillomandibular expansion). This option requires a combination of orthodontic appliances and surgery to expand the jawbones, with the goal of enlarging the airway and increasing the space available for the tongue.
- UPSIDE: Make room for the tongue in the mouth. May reduce obstructive sleep apnea.
- DOWNSIDE: Loss of sensation to the front face around the mouth, a risk of postoperative dyspnea due to pharyngeal edema, and some aesthetic dissatisfaction, gapping in the front.

9. Bariatric Surgery: Excessive weight or obesity may be a major contributor to a person’s OSA. Weight gain can cause fat tissue to build up around the throat and at the base of the tongue. Medical weight loss or bariatric surgery may be indicated in certain cases.
- UPSIDE: You get skinny really, really fast! (May reduce obstructive sleep apnea.)
- DOWNSIDE: Excessive bleeding, Infection, Adverse reactions to anesthesia, Blood clots, Lung or breathing problems, Leaks in your gastrointestinal system, Bowel obstruction, Dumping syndrome, which leads to diarrhea, flushing, lightheadedness, nausea or vomiting, gallstones, hernias, low blood sugar (hypoglycemia), malnutrition, ulcers, vomiting, acid reflux, the need for a second, or revision, surgery or procedure, Death (rare).

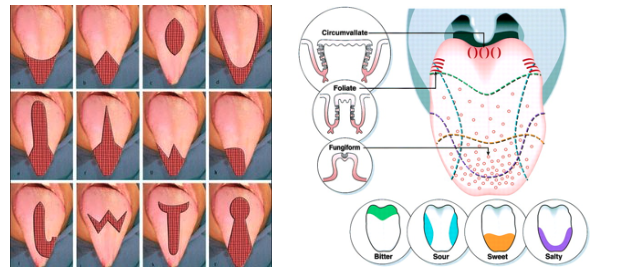
10. Tongue reduction surgery may be helpful when the tongue is abnormally enlarged. Reducing the size of a person’s tongue may cause the airway to collapse less, thus improving airflow and breathing.
- UPSIDE: Tongue has been reduced in size, and may reduce obstructive sleep apnea.
- DOWNSIDE: bleeding, hematoma of tongue base, abscess of tongue base, altered taste, tongue numbness, deviation of tongue extension movement, dysfunctions of pronunciation of wards and swallowing. Which taste buds do you want to sacrifice?
Get non-surgical sleep apnea treatment in Utah
So, before we resolve ourselves to sleeping poorly, being unproductive, or even worse, having something cut out of our body, be assured there is a better way with our holistic treatment for sleep apnea.
At the very least, you should sleep on it. To learn more about our procedure for our alternative sleep apnea treatment, check out this post.
