Sleep Apnea Specialists
Obstructive Sleep Apnea Treatment
Common Symptom Clusters Suggest a Common Causal Relationship
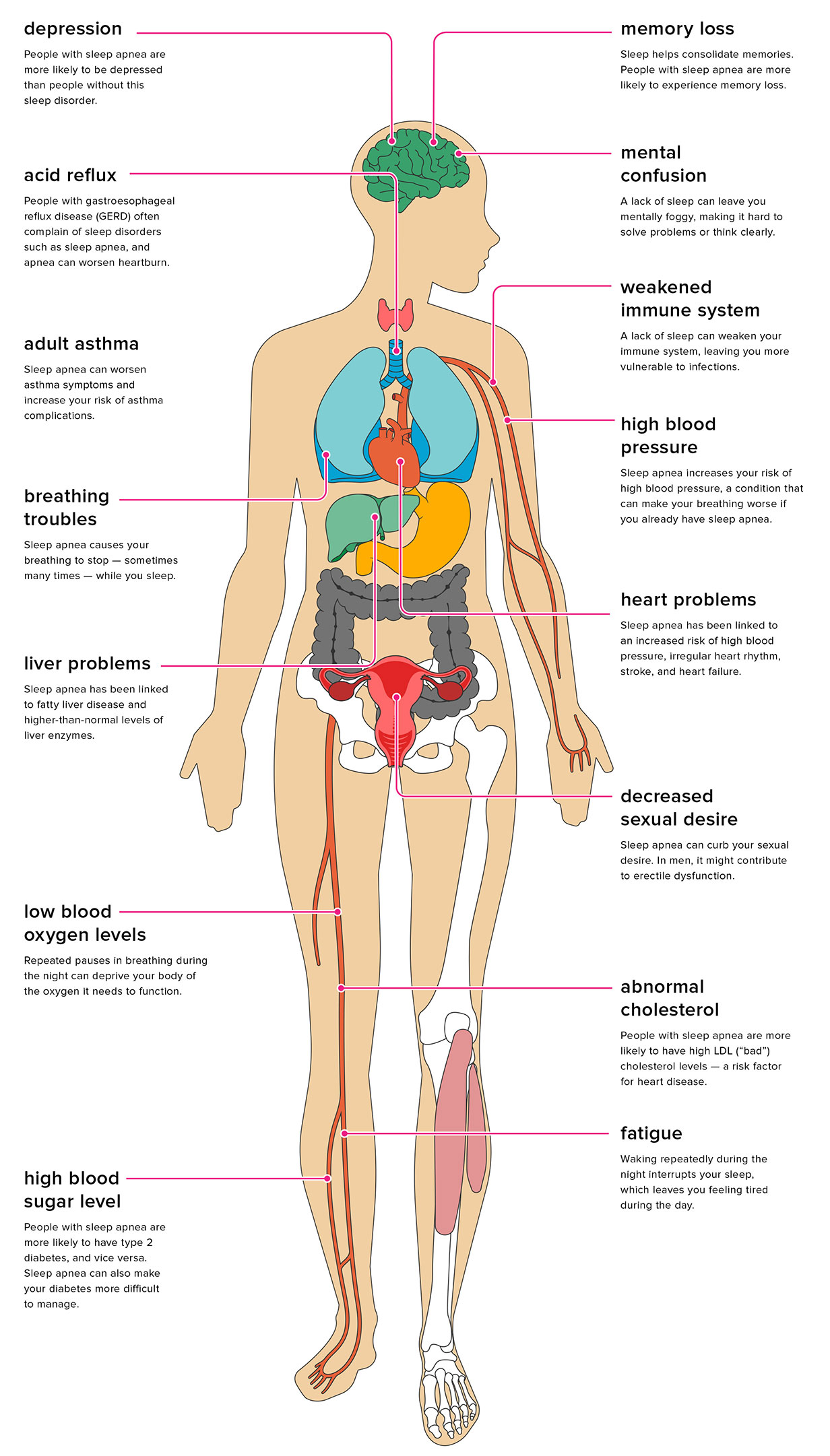
The far-reaching effects of obstructed sleep breathing can stagger the mind. Copious research shows that obstructive sleep apnea, the most common sleep breathing disorder, is clearly linked to other serious disorders and harmful health conditions.
As a sleep apnea doctor who regularly treats sleep disordered breathing, improving sleep breathing and the quality of sleep has become my greatest clinical concern for both the long or short term health status of our patients. When obstructive sleep apnea and other chronic conditions are present, all conditions improve or resolve proportionately when the underlying cause of sleep apnea is addressed and treated.
Amongst health practitioners who are informed about the risks of Obstructive Sleep Apnea, it is common knowledge that most known medical conditions are worsened when Obstructive Sleep Apnea (OSA) or Central Sleep Apnea (CA) is present. A study published in the journal Sleep, as early as 2008 reported that people who have severe sleep apnea involving more than 30 breathing pauses per hour during sleep, have three times the risk of dying due to any cause compared with people who do not have sleep apnea. 3X the risk of dying due to any cause! When I first read that statistic it got me thinking about the causes of sleep breathing disorders and what could possibly go wrong. It seemed that much of the research at the time pointed to obesity as the cause. As it has turned out, obstructive sleep apnea afflicts way more of the earths population than those who are overweight.
Breathing is fundamental to life, and without this vital function, we die! I began to study the bodies control centers that manage and regulate the entire respiratory system. As I delved deeper into the understanding the complex mechanisms of respiration, I discovered that the primary control centers for respiration are located in the central nervous system at the level of the throat and upper airway in the cervical spinal cord, the brainstem, medulla, pons and midbrain. Right where the head sits on the top of the neck!
It has been a long road of discovery for me, and not just for me. There have been many researchers and clinicians from diverse disciplines who are discovering causal links between all Disease and sleep disordered breathing. As I share with you my observations, my hope is that it will give you a useful understanding of how powerful breathing disorders are, and the massive effect that have on our body, and common this condition has become in our modern American society.
Craniocervical dysfunction appears to be related to obstructive sleep apnea. In many specific cases, craniocervical dysfunction appears to be a causative condition that when corrected dramatically improves or resolve sleep apnea entirely. Therefore, as my experience would suggest: obstructive sleep apnea and central sleep apnea share the common condition of craniocervical dysfunction. Correcting a primary attribute of craniocervical dysfunction occurs when we remove the atlas subluxation, and this directly and immediately improves pharyngeal function. It would seem therefore that the atlas subluxation complex could be a significant causative or contributory factor of disordered sleep breathing diseases, as well as those symptoms and conditions mentioned below.
Some things to keep in mind. True sleep apnea specialists who understand all of the causes and health implications don’t exist. We have experts in sleep science, and breathing science but sleep disordered breathing, while narrow in its title, accepts many successes from in its diversity of interventional specialists; Just to name a few, dentists, craniocervical chiropractic specialists, physical therapists, chemist’s, dieticians, orofacial therapists, medical device manufacturers, orthotists and implantologists all make some sort of contribution to solving the ubiquitous problem of obstructive sleep apnea.
When we think of a Sleep Apnea Specialist, it’s important to consider how we are conditioned to think of medical specialities. In this instance, a sleep apnea specialist is one who has been trained in the provision of certain drugs, or medical devices like CPAP or BiPAP which are designed to force air under continuous or alternating pressures through the partially or completely obstructed pharynx, or those who find solutions at the end of a scalpel. While some sinus, upper airway, pharyngeal, glossal or oral revisions can be useful and very beneficial, most are short-sighted and provide diminishing returns over time. We bring a natural, non-invasive and highly successful treatment option to the table. Our corrective system not only improves sleep breathing, but also “wake” breathing. People feel better, sing better, run further, have better balance, and get more out of their life.
In the instance of PAP machines, while there is some immediate good that results from an artificial breathing machine, but it should not be looked upon as a universal cure or even a viable and sustainable treatment without its own risks. It is, in the purest sense, an emergency use device, a heroic temporary solution to be relied upon until the underlying problem is solved or notably improved so as to minimize any future harm or risk.
The research and science suggest that there are many risks in the permanent use of PAP (positive air pressure) devices which adversely affect our central nervous systems breathing control centers, and potentially harm the health of mucosal membranes of the nose, mouth and throat as well as aspects of our oral health. Further risks develop after prolonged use of certain masking straps and fittings causing subtle shifting and compression of facial bones, congestion of craniocervical venous drainage at the back of the skull and top of the neck, the face, eyes and cheeks and under the jaw. (Ironically, the compression of the elastic straps increases the compression effect on the airway restriction point where the obstruction takes place!)
Surgeons who treat sleep apnea use nip and tuck techniques to revise the upper airway, altering or removing vital tissues which are critically important to our long-term air filtering systems, which vanguard our immunity. It is not ideal to trim away at the tissues that condition and filter the air we breathe to protect our respiratory system, or rely upon to swallow food, water or saliva, or act as the first line of defense to both our digestive and respiratory systems. Our respiratory system and our digestive system share a common portal called the pharynx that leads to the great mystical “inside of our body”. Surgically altering structure alters or removes the vital function of that tissue. Physicians take an oath that remind us that while trying to help cure our patients of disease and disorders, we shall do no harm. We should be reminded that while some sinus, upper airway, pharyngeal, glossal or oral surgical revisions can be useful and beneficial, most are short-sighted and provide diminishing returns over time.
Other sleep apnea specialists implant medical devices that create a tongue thrusting movement throughout the night when an obstructive event is detected by a computerized device. This device cleverly mimics and produces a human behavior known as a tongue thrust, because a tongue thrust advances the tongue forward. Our central regulating system do this naturally when oxygen drops, producing a “night-time clenching or grinding mechanism which we call Sleep Bruxism” Learn More. The implanted muscle stimulator embedded in the genioglossus muscle (tongue thrust muscle), like the bodies bruxism mechanism pushes the tongue forward removing the oropharyngeal obstruction. Traditionally, a tongue thrust was thought to be a pathological disorder, but now is being electronically stimulated to treat obstructions. While bruxism has stood the test of time, implanted devices have not. In other words, Sleep Apnea Specialists use techniques and devices that are invasive, and the procedures and processes don’t always work, and often come with harmful side-effects. Side effects which can be as dangerous as the condition they are trying to treat.
There is safer and effective way that is science based and clinically tested. We think it’s better because there are no adverse effects or events, and outcomes are very positive. We have helped thousands of people sleep better, breathe better and live more healthy, productive and enjoyable lives.
There are several important health conditions that seem to be directly related to obstructive sleep apnea and often accompany the primary compliant of sleep apnea as concomitant complications.
Sleep Apnea Concomitant Conditions
Depression and Anxiety are worsened as the brainstem, and limbic systems are deprived of oxygen and exposed to lingering CO2 saturations. Depression can be worsened as venous blood is congested at the craniocervical junction through an atlas displacement. CO2 concentrates in the brainstem, frontal lobes and limbic system, and these brain tissues and their functions are adversely affected. The same atlas displacement that compresses the internal jugular vein can disrupt vagus nerve tone, and imbalance heart regulation, increase our anxiousness and up-regulate the “fight-or-flight” response, and can further affect the pharynx and esophagus.
Our Fix: The TAP Procedure opens the spinal fluid channel between the brain and spinal cord, can decompress internal jugular vein restrictions caused by the subluxated atlas, and take pressure off the vagus nerve at the craniocervical junction where those structures exit the occiput. The results can be immediate and life-changing, affecting the way you feel and function.
Acid Reflux can become chronic (GERD) in the presence of Obstructive Sleep Apnea. Lax pharyngeal muscles lie at the root of esophageal regurgitation because lax pharyngeal muscles tend to cause apnea obstructions. As the body unsuccessfully tries to pull breath (air) into the chest from the outside against the resistance created by the obstruction in the pharynx, the vacuum created in the chest cavity from the muscles of respiration under the conditions of recumbent sleep allow the acidic gastric contents to be siphoned upwards through the lower diaphragm sphincter muscles into the esophagus and upwards into the base of the throat to our swallowing and breathing junction. When we awaken to the taste of acid from heartburn in the back of our throats, we may know that our gastric contents have completed their journey up the esophagus and have entered the lower pharynx. Since all obstructive apneas are caused by obstructions in the pharynx, when air intake is obstructed from being pulled into the lungs in the chest cavity, the body’s respiratory effort pulls gastric contents up through the esophagus towards the pharyngeal restriction.
Our Fix: The TAP Procedure helps resolve esophageal reflux by lowering obstructive events. This is done when the atlas subluxation is removed and a subsequent increase in the tone of the pharyngeal muscles allows the airway to remain patent (open) while sleeping. The nerves that control these important muscles of swallowing and breathing come directly out of the central nerves located in the craniocervical junction. A properly functioning craniocervical junction keeps the airway open while sleep breathing, and allows gastric contents to stay below the lower esophageal sphincter where they belong.
Neurodegenerative Diseases:
Alzheimer’s Disease (AD) more than doubles in the presence of Obstructive Sleep Apnea. 40% of Alzheimer patients have been diagnosed with the comorbidity of Obstructive Sleep Apnea, but the results of some studies suggest that the actual number of AD patients with OSA is likely much higher.
Parkinson’s Disease (PD) patients have been shown to actually improve when their Obstructive Sleep Apnea is treated with CPAP. Heart Disease in these patients have a reversal of heart damage after one year of effective intervention.
Multiple Sclerosis (MS) patients often suffer from disordered sleep breathing. Clenching and grinding of teeth can exacerbate the trauma to the brain and venous drainage system as the temporal bone mobility radically increases. Research has shown the temporal bone associated with TMJ to be 600% more unstable in MS and ALS patients. This excessive mobility can affect the internal jugular vein drainage efficiency, cause venous pooling in the critical venous system that cleans the brainstem, and is thought to be a causative contributor to the periventricular white matter lesions found in MS.
Memory Loss, Foggy Thinking, Mental Confusion and Fatigue often come as a package deal. That is because these symptoms often stem from a common cause. When they do, that Common Cause can also lay at the origin of Sleep Disordered Breathing. These symptoms when clustered together, I have come to see as an early warning sign of impending neurodegenerative disease. The more retrospective studies we undertake, the more we are able to understand about the early warning signs of neurodegenerative disease. This is why we claim the TAP procedure to be neuroprotective.
Our Fix: The TAP Procedure aligns the spinal fluid channel between at the craniocervical junction and allows the cerebrospinal fluid to flow into and out of the craniocervical junction intermittently with breathing in and breathing out. Twists and turns in the atlas-axis skull base can directly restrict the normal movement of cerebrospinal fluid, and since CSF movement into and out of the cranial vault is the primary mechanism of clearing metabolic wastes from the brain, impedance of this mechanism is tied to brain disease.
Note: CSF movement from the spinal column moving into the skull is the primary brain cleaning mechanism which keeps the metabolic debris from building up in the brain tissues. The brains of patients suffering with dementia exhibit excessive build up of metabolic debris that is not present in patients without dementia. Craniocervical dysfunction and misalignment can interfere with the “brain drain” by stifling internal jugular vein blood flow and impeding cerebrospinal fluid movement. Jugular impingement and cerebrospinal fluid restrictions have been shown to exacerbate all neurodegenerative diseases.
High Blood Pressure and Heart Disease have long been related. Research has shown that Obstructive Sleep Apnea increases the likelihood of both. High blood pressure (hypertension) often belies heart disease. That is why hypertension is called the silent killer. Since Obstructive Sleep Apnea more than doubles the incidence of high blood pressure, we may consider OSA the guilty accomplice of high blood pressure.
Our Fix: The TAP Procedure can reduce High Blood Pressure in patients. According to a double blinded cross-over study published in the Journal of Human Hypertension in 2007, transdermal atlas positioning reduced the blood pressure equivalently to 2 blood pressure medications, combined. That means that having the TAP procedure performed provides the same cardio-protective benefits without the toxic pharmacological side-effects.
Low Oxygen Levels can become chronic and occur when respiration (breathing in and breathing out) is limited. This occurs when we are awake and when we are sleeping. That means that the problem is also part of wake breathing as well as sleep breathing. When the atlas and axis are measurably misaligned under the skull, it can adversely impact the nervous system control centers that govern the basic functions of breathing and swallowing. The upper airway, known as the pharynx can become restricted and narrowed. This creates chronic low O2 levels and chronically high systemic acidity as CO2 breaks down into carbonic acid and does not escape adequately through exhalation.
Our Fix: The TAP Procedure opens the minimum cross sectional area of the pharynx, the location where over 99% of the obstructions occur in OSA. This increases the overall O2 saturations present in the blood at any given time. The result is better overall circulation, muscle tone and brain health.
If you are suffering from sleep disordered breathing and are looking beyond the stop-gap benefits of CPAP, or if you are suffering from any of the conditions listed above and feel that your sleep quality is interrupted by startling awake, gasping for air or snoring, I encourage you to reach out and have a genuine conversation with our new patient advocate who can answer your individual questions and explore with you whether a consultation is in your best interest.
Request Consultation
Fill this out and we will be in contact with you
"*" indicates required fields