Whiplash is becoming one of the most common injuries in modern civilization. The reason for this is the increased number of car crashes, contact sports trauma and the growing presence of connective tissue disorders in our normative population! Whiplash, historically known as cervical acceleration deceleration injury, is often dismissed as “a no big deal injury” with little long term consequences by insurance companies’ business practices and perspectives. Studies have been funded by the insurance companies outcomes and effects of whiplash. The tone and tenor of these studies tend to de-emphasize effects of these “minor” soft tissue injuries.
There is a cornucopia of well-researched, well-designed studies to demonstrate mechanisms and effects of actual damage from whiplash injuries–whether from high or low speed collisions. More particularly, the impact of these mechanisms and effects concentrate the negative effects to the lower-mass of the craniocervical junction zone and raise the likelihood of damage to the supportive ligaments and structures that once weakened, allow altered blood flow patterns which can further disrupt the cardio-respiratory cycle. A cascade of functional derangement may ensue, including disruption of cerebrospinal fluid dynamics, interfere with spinal cord, nerve and and brainstem function and a noticeably weakened and altered postural system.
What is the principal mechanism of injury from an upper neck whiplash?
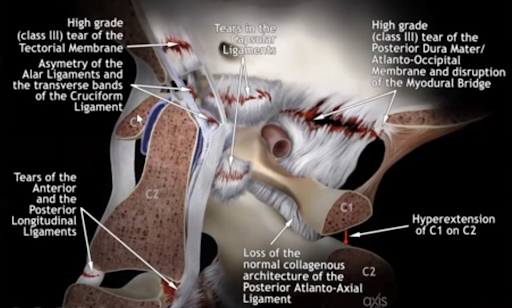
It’s the speed. The accelerating stop or start, back and forth or side to side, can tear the core stabilizing ligaments of the craniocervical junction. This destabilization can result in chronic misalignment of the upper cervical spine, and as such, may not tolerate therapeutic manipulation well. The upper cervical spine consists of three vertebrae and one skull bone. The C3 (root) C2 (axis) and C1 (atlas) spinal vertebra function as highly mobile support structures for the C0 (occiput) also known as the base of the skull. Critical ligaments in this region that preserve normal and safe movement of the head on the neck can be torn, stretched and damaged with whiplash injury. The cross-sectional image seen below shows the central core of C0, C1 and C2 sustaining our head while visually illustrating a few of the structures that can generate pain when damaged.
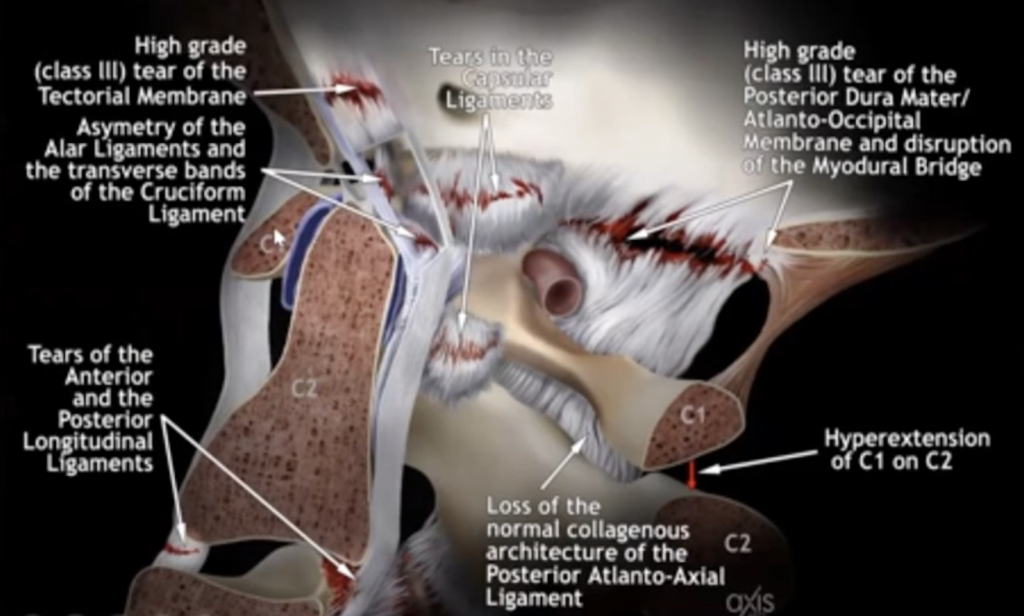
Whiplash Injury may Tear Ligaments and Membranes of the Craniocervical Junction
It is my opinion that intervention to this region following a whiplash injury should be performed judiciously. Transdermal Atlas Positioning with image guidance, also known as the TAP procedure can be quite effective in gently and precisely reordering the constituency of craniocervical elements to a normal, higher functioning state. The TAP procedure uses a robotic-armed instrument developed through a collaboration effort with the Sweat Institute and Georgia Tech, along with the innovations of a 2D and 3D guidance image sequence and bite registration technique developed by Dr. Christopher Chapman. The procedure itself is painless and brief, and comes with no known adverse events. Results can be felt immediately in most cases. Imaging and measurements are performed both before and after the procedure and confirms a successful procedure, or, provides “course-of-care” correcting guidance.

TAP re-aligns the head and neck following Traumatic whiplash injury. The TAP (Transdermal Atlas Positioning) instrument enables a doctor who has been trained and certified in the Atlas Orthogonal procedure to precisely and gently reposition the atlas vertebra into its proper position without further injuring the delicate structures of the craniocervical junction. See and illustration of how the TAP procedure corrects the head and neck injury following whiplash
Automobile accidents, or car crashes can cause whiplash. In fact, it is rare that one will escape even minor car crashes without some form of whiplash damage. When you consider the physics of it, it becomes clear that it’s not so much the rate of speed at the time of injury, but rather the the rate your speed changes (“change in velocity”) over very short periods of time from in-motion to stationary, or from stationary to motion that provides the harm. Rate of speed change is the culprit! For example, it is quite thrilling to accelerate in a sports car from 0 to 60 mph in under 3 seconds. We can do this without damaging the ligaments and structures that stabilize the spine. However, if we accelerate from 0-6 mph in a mere ¼ of a second, we will potentially tear loose critical ligaments that stabilize the head and neck. These are the typical circumstances in a “low speed”, rear end collision. Our connective tissues behave like silly putty, because they have a viscoelastic quality. If abruptly stretched, silly-putty rips… if stretched slowly, it yields without tearing.
Low speed rear-end car crashes cause more damage than you might think. If you’re unfortunate enough to have been in one of these recently or in the distant past, you may have felt just fine at first. Perhaps not so good a few weeks or months later when you started to feel discomfort or pain in the neck and shoulders. Pain and discomfort may have come on “out of the blue” weeks or months after the car crash. Maybe the crash wasn’t even reported to your insurance. That makes sense, because the damage to your car was minimal, and you thought there was no damage to you! You probably didn’t understand the delayed onset risk, and so you probably didn’t associate the little fender bender with symptoms that came on some time thereafter.
It can take time to start feeling symptoms from whiplash injury. The reason is– it takes time for structures like muscles and fascia to become symptomatic after a core ligament injury, because it takes time for muscles to chronically fatigue and once the primary stabilizers (ligaments and other connective tissues) are torn or incapacitated. It’s how the body is designed to maintain protection and function after primary injury. It can shift function to other areas to maintain essential processes, like movement. As these compensating muscles reach their limit, they begin to adapt to the lack of support of the core stabilizers of the head and neck junction, and this adaptation process is primarily where the pathology and pain comes into play–pain and inflammation, spasm and trigger points–often a good distance in time from the initial injury. There may be minimal damage to your car’s bumper, but damage to your spinal structures can only be determined by advanced images. Or, symptoms that set in over time.
Damage to the critical ligaments that protect the nerves and blood vessels which cross the head-neck junction can be the source of post-whiplash pain syndromes. When these tear, the “work” of stabilization is taken up by the muscles of the head, neck and jaw.
Whiplash injury to connective tissue structures shown above such as the accessory, alar, apical or transverse ligaments… Or, the tectorial membrane or other crucial membranes that cross the junction can cause headaches, neck pain and migraines. Yes, headaches, neck and jaw pain may come from damage to these core connective structures, as well as compressed or injured blood vessels such as the carotid and vertebral arteries. Injury to any of these structures may be difficult to diagnose because they ARE situated near the core of the body, and occupy the transitional zone between two important anatomical regions–the head, and the neck. Unless specific advanced imaging protocols are utilized to diagnose them, they often go undetected and undiagnosed.
Traditional imaging study protocols usually select either the head, or the neck, or perhaps both, but not the vital transitional zone interconnecting the two regions. You would think that when your doctor orders brain and cervical MRI’s that you would see clearly any potential symptoms causing damage, but that is simply not the case. After reviewing hundreds of adjacent imaging sets on symptomatic patients, I have found more often than not, incomplete visualization of symptom causing structures. There is enough credible research in peer reviewed and medically indexed scientific journals to assign the head and neck transitional region its own special imaging series called the Craniocervical Junction Imaging Sequence. If you don’t get this study, and your injuries are in this area–they won’t get identified and documented, therefore you will miss important objective imaging facts and features that can explain your symptoms.
Several of these important ligaments, such as the alar and accessory ligaments, along with the tectorial membrane are thin enough that unless the ordering physician calls for these special imaging sequences in this “in-between” transitional boundary, relevant findings will be missed entirely, and the patient’s symptoms will remain unexplained and undocumented.
While injury here is often overlooked, with the right imaging approach, an important injury can be observed and identified with the right MRI order and radiology assessment. Once identified, a craniocervical junction specialist can then diagnose and potentially offer remedial treatment. Since the ligaments and connective tissues at the core of the head-neck junction are pain generating structures if damaged, an explanation for migraines and headaches, occipital pain and a plethora of other global dysfunctions can be offered.
I have seen many cases of patients who underwent whiplash trauma from minor rear end collisions who have continued to suffer after seeing very competent and well-intended chiropractors, physical therapists, massage therapists, and pain management specialists. None of these clinicians have been able to identify and resolve the underlying cause of the patients chronic pain and suffering. If this is your situation, then you may need a specialist in chiropractic craniocervical junction procedures, where this vital center may receive the care it needs to really begin to heal.
We have performed the Transdermal Atlas Positioning procedure on hundreds and hundreds of whiplash patients and had immediate results. In most cases the symptoms that have been plaguing them for months, and even years, immediately begin to clear and the injured structures begin to heal.
Helpful Tips:
- You are not your car, and you do not share damage levels with your car! This means that just because your car is not badly damaged does not mean you haven’t sustained internal damage to these critical ligaments at the head and neck junction.
- Get the right imaging soon after the accident. When the body tissues are injured they immediately go through the natural process of healing and forming scar tissue. Getting advanced imaging within the first 30 days allows the injury to be more readily detected with certain MRI techniques. When detected early, it serves as legal documentation that differentiates fresh injury from pre-existing damage.
- Get an expert opinion on the craniocervical junction region. If you’re suffering from pain following a whiplash injury, come in for an assessment, and we will take images of your craniocervical junction and help you figure it out.
- Don’t give up your search for answers! We often see signs on our 3-D imaging signs of damage to the supportive ligaments and connective structures of the craniocervical junction that were missed. If we suspect this, special MRI’s can be attained even years later that can help us understand the original injury and start your healing journey leading to repair and stabilization.
The Lift Clinic’s special imaging to determine problems at the head-neck-jaw junction.
If your case is with an attorney, or you have long since settled, we can re-position these craniocervical junction structures and provoke healing with our TAP procedure.
The transdermal, atlas, positioning procedure is safe and effective at restoring the craniocervical junction, and not injuring further, the supportive and delicate vascular structures in this region. we have done this procedure thousands of times and helped hundreds and hundreds of car crash victims get back on the road to recovery.
Peer reviewed open-access Chapter on Craniocervical Junction Syndrome
Excerpts, “at-a-glance”
Craniocervical and Atlantoaxial Junctions and the Effect of Misalignment on Cerebrospinal Fluid Flow. S Rosa, J Baird, D Harshfield and M Chehrenama
Abstract
“The craniocervical junction (CCJ) is comprised of the inferior surface of the skull, the atlas and axis, as well as muscles and connective tissues that attach the skull to the cervical spine. The CCJ encloses the central nervous system (CNS), encephalic vasculature and the cerebrospinal fluid (CSF) system. The CCJ spans the brainstem to the spinal cord, including the vascular system as well as connecting the cerebrospinal fluid (CSF) cisterns within the skull to the CSF channels in the spinal canal. Malformation and misalignment of the craniocervical junction can cause a constellation of cerebral and other neurological signs and symptoms collectively called craniocervical syndrome (CCS). The signs and symptoms of craniocervical junction syndrome may be due to mechanical strain causing deformation of dura mater, vasculature and other structures of the cranial vault resulting in irritation of and dysfunction of affected tissues. Deformation of the CCJ may also obstruct blood and CSF flow. Chronic ischemia, edema and hydrocephalus can cause degenerative cascades that can in turn lead to neurodegenerative diseases.”
